
Giant Dog Breeds (90+ lbs): A Complete Guide
Highlights: Giant breeds are considered breeds that weigh over 90 pounds. Caring for and raising a giant-breed dog requires space, training, and attention to your dog’s special needs. Giant breeds
Published by
Crowder SE, Berg M, Bellows J, Artzer M, MacGee S and Schultz L.
Periodontal disease prevalence in dogs has been well established and is an under-treated pathological condition in dogs. The development of the pellicle, the role of plaque and the presence of calculus in dogs and its association with periodontal disease have been extensively described in the literature. Pellicle development forms within an hour after prophylaxis and hours after tooth eruption. The sequence of plaque formation involving early bacterial colonization occurs within 6 hours and plaque maturity in 48 hours with the incorporation of minerals from the saliva to maturation into calculus.1 The development of halitosis and gingivitis resulting from inflammatory mediators and the release of chemicals may progress to periodontitis. The hallmark of chronic periodontitis being the degradation of the periodontium leading to attachment loss and eventual tooth loss. The development of periodontal and endodontic lesions can result in abscessation, mobility, pain, and tooth loss.
Previous research has demonstrated that education is paramount to client compliance with tooth brushing and other measures to prevent the progression of periodontal disease. The educational model used in human plaque control consists of patient education regarding the incidence and cause of periodontal disease, demonstrating “in -office” plaque control methods, primarily tooth brushing, and directing patients to other devices like floss or flossing products (flossers), mouth rinses for chemical calculus retardation, anti-microbial benefits and xerostomia, gels, chewing gum, and other plaque control measures. At-home brushing in a dedicated subpopulation of dog owners revealed that only 47% were brushing weekly after six months or more after receiving client education and brushing demonstration.2 Numerous products are available for dental and oral health over-the-counter and online for pets with claims for fresher breath, “clean teeth” reducing calculus and controlling plaque or “promoting oral health” with no required evidence to market those claims. In 1997, The Veterinary Oral Health Council (www.VOHC.org) was established to recognize products that meet a defined standard of calculus and plaque retardation or reduction in dogs and cats. 3
Client compliance with the gold standard of brushing has typically been low and incorporating a daily dental hygiene chew has resulted in reduction of calculus, less gingivitis and decreased periodontal bone loss. 4 Another study determined that feeding a daily dental hygiene chew six days a week reduced calculus deposits and promoted periodontal health.5 Halitosis is a common complaint of dog owners affecting all breeds. Without client education on the etiology and signs of periodontal disease, owners may only identify oral pathology by malodor. Oral malodor of the oral cavity often motivates clients to seek veterinary care for their pets.Oral malodor is associated with periodontal disease commonly affecting dogs and cats. 6,7 The stage of periodontal disease along with the increasing levels of volatile sulfur compounds (VSC) has been reported as playing a role in possible collagen destruction and membrane permeablity.6 The dental chewa used in the current study has a unique honeycomb design developed to provide an interdental mechanical removal of calculus and plaque with “flossing” action. The chew also has ingredients that have been shown to provide chemical retardant of plaque and provide anti-oxidants including Yucca schidigera extract, zinc oxide, and vitamin E.
This study aimed to evaluate the efficacy of a honeycomb shaped dental chew in reducing hardened calculus, plaque, gingivitis, and malodor in client owned dogs in their normal home environment including various breeds, skull types, ages, and weights. Calculus, plaque, gingival and malodor scoring were performed under sedation and evaluated under general anesthesia after 60 consecutive days of receiving a daily honeycomb shaped dental chew treat. The patients also received additional periodontal probing, an oral evaluation under anesthesia, and professional dental prophylaxis at the second evaluation.
Thirty-two canine patients were screened for enrollment. At initial consultation (Day 0), the study protocol, methods and materials, and expectations of the client with required visits were discussed with each owner. Clients were instructed when scheduling the initial consultation to fast their dog for 12 hours from food, but water was allowed ad libitum until the admittance appointment time. Clients received a study letter outlining the protocol and follow-ups visits. Clients signed an informed consent and waiver form outlining the study protocol and expectations. Ingredients were listed and acknowledged by client that there were no known allergies to ingredients. Enrollment was voluntary and clients informed that patients would receive a complimentary dental prophylaxis at the end of the study. If the patient met the inclusion criteria, they were asked if they would like to be included in the study. Clients consented verbally and with written consent for the duration of the study to “not use any home dental care products like toothpaste, rinses, dental chews, or direct application of any dental products while enrolled in the study including toothbrushes, finger brushes, wipes, and other gels.” Clients acknowledged the statement “My pet’s diet will remain the same and no changes to the diet will be made while enrolled in the study. I understand I will give my dog one Yummy Combs® a day for supervised chewing and ingestion. I will not give any other hard treats, toys, or dental treats/chews.” Each dog served as their control with a single subject design with each dog serving as a baseline for Day 0 and data compared against their own habits/anatomy, and biological environment.
One patient was excluded at initial enrollment due to an oral tumor detected in the caudal maxilla. Another patient withdrew from the study due to a diagnosis of lymphoma after Day 0 scoring.
Patients with advanced periodontal disease (stage IV) and enamel hypoplasia were excluded (2 dogs). During the intake and admittance appointment for the second evaluation, one owner noted that they fed the chew less than 50% of the recommended times; this patient was withdrawn for non-compliance.
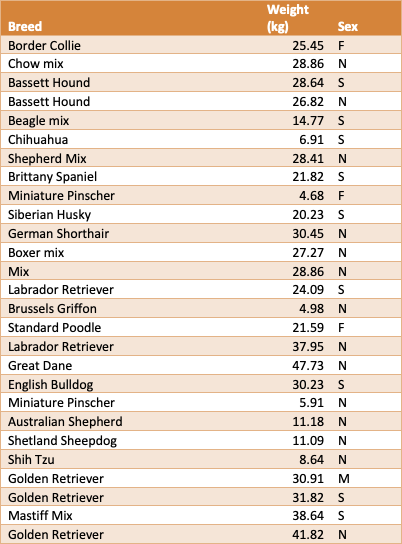
Twenty-seven client owned dogs completed the study with over 25 different breeds. The mean age was 6.1 years with weight ranges of 3.72 kg to 47.73 kg (mean weight was 23.69 kg/52.12 lbs.). Environment remained unchanged with indoor housing typical of client-owned dogs. There were 24 normal occlusions (Class 0), 2 Class III malocclusions and 1 Class II malocclusion represented in the study.
Inclusion criteria were visible calculus on teeth with a physical exam indicating patient was stable for sedated exam and general anesthesia. Exclusion criteria included any dog with a current diagnosis or history of cancer, uncontrolled metabolic disease, autoimmune, or immunosuppressive disease, stage IV periodontal disease or mobile teeth that prevented the enrolled dog from chewing a dental treat. Dogs that received a dental prophylaxis within the last 24 months were also excluded.
Seventy-four (74%) of the dogs had never had a professional dental prophylaxis or dental procedure and of the dogs that never had a dental procedure the dental prophylaxis free (DPF) time range averaged 5.7 years. Of the 7 out of 27 (26%) that had received a dental prophylaxis prior to enrollment, the average time since any dental procedure or prophylaxis was an average of 4.1 years (DPF-4.1 years). Patients included 15 male dogs (one intact M, fourteen neutered N) and 12 female dogs (three intact F, nine spayed S). Table 1
Day 0: First consultation: initial screening, patient history, physical exam, rectal temperature, heart rate, and respiratory rate (TPR), body weight, a conscious oral exam, sedation and calculus, plaque, malodor, and gingivitis scoring.
Dog receives Dental Treat based on weight daily for 60 days.
After Day 60 (+/-10 days): Patient history, physical exam, general anesthesia, calculus, plaque, gingivitis and malodor scoring, and dental prophylaxis. Although due to scheduling client-owned dogs some were within +/- 10 days of the 60 day timeline, it will be denoted as Day 60 for the second evaluation under anesthesia.
Grading criteria were used following VOHC grading guidelines measuring calculus, plaque and gingivitis.1,5 Dental scoring was performed by the same trained grader for all dogs and both days Day 0 and Day 60. The teeth scored included 103,104,107,108,109, 203,204,207,208 and 209. (noted as mandibular I3, C, PM3, PM4, MI) and 404,407,408,409,304,307,308,309 (noted as maxillary C, PM3, PM4, M1).
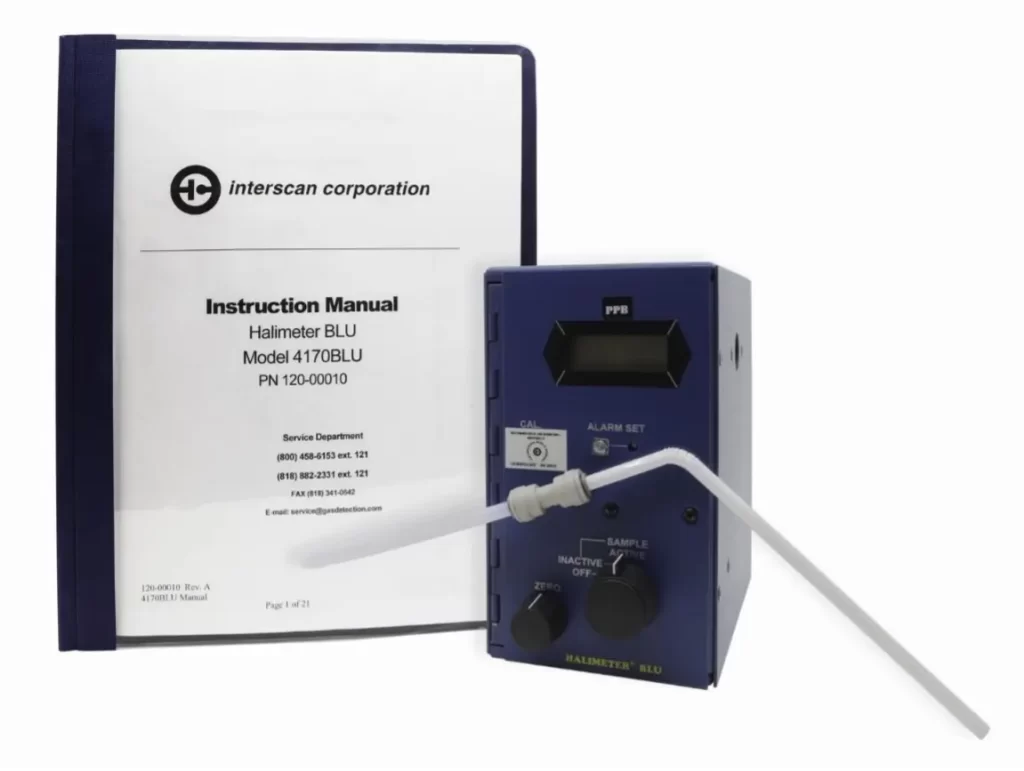
Medetomidine and vatinoxam hydrochlorideb were used with the recommended manufacturer dosing by weight with an intramuscular injection for sedation. If additional sedation was needed to achieve lateral recumbency and relaxation, methadonec was added at 0.2 mg/kg. Methadone was added for 30% of patients to provide additional sedation for scoring (9/30). Twenty-one of the thirty patients (70%) evaluated on day 0 for a sedated exam had adequate sedation with medetomidine and vantinoxam hydrochloride for scoring. Subjects were transferred to a dental operatory for scoring. A portable halimeterd was used for measuring volatile sulfur compounds (VSC) and quantifying malodor numerically (Image 1) for each patient. A clean plastic straw extensione was added to the halimeter for each patient and centered in the buccal area near the maxillary 4th premolar without touching any anatomy. The halimeter was prepared by allowing the unit time to recalibrate before use. Each patient was measured three times and a mean malodor score was calculated and recorded. The halimeter reset to 0 before the next measurement was taken. Malodor was scored first prior to intubation, when possible, to avoid dilution of VSCs or change in VSCs while handling and scoring the other indices. Gingivitis was scored using a modified Loe and Silness index.1,3 Calculus was graded on two criteria, coverage and thickness using a modified Schiff method and a whole tooth score. 5 Plaque was assessed using the modified Logan and Boyce Index with an air water syringe on a dental unitf and an ultra-violet light to aid in visualizing coverage8,9.
Intra-oral photos were taken of the buccal surfaces of each patient’s right and left sides with check retractiong. After scoring by a trained experienced grader and readings recorded, patients were transferred to padded recovery cage, directly supervised and monitored until standing and sternal.
Patients were monitored while under sedation with EKG, heart rate, oxygen and end tidal CO2 levels with documentation of blood pressure with a multiparameter monitor. Visible dental pathology including missing teeth, discolored teeth, gingival recession, fractured teeth, and other pathology was recorded to be addressed at a future appointment. One patient was noted to have halitosis secondary to a large black pigmented oral tumor and patient was withdrawn from study.
At discharge appointment owner was given a compliance calendar to check off each daily treat given and consumed. Each client received a new 60 day supply bag of the honeycomb-shaped dental chews based on patient’s weight, emergency contact numbers, and verbal and written instructions on administering the chew under direct supervision.
After 60 consecutive days of administration of the daily Honeycomb shaped dental chew, the patient returned for repeat scoring and recording indices. At the Day 60 (+/-10 days) visit, clients were instructed to have patients fasted 12 hours from food, but water could be offered ad libitum until admittance appointment time. Dogs received a physical exam, awake oral exam, TPR, body weight and premedication with maropitant.h Based on the sedative response of Day 0, anesthesia protocols were adjusted for adequate sedation for each patient. For patients that did not achieve adequate sedation on Day 0 with the addition of methadone, dexdomitori was substituted in 4 dogs where more sedation was desired from the Day 0 sedation protocol.
An area over the cephalic vein was shaved, aseptically prepped and placement of an intravenous catheter for fluid administration. Lactated Ringersj was administered at 5mg/kg/hour during the evaluation and grading. Anesthesia was induced with propofolk to effect, subjects orotracheally intubated and maintained on isoflurane.l Eighty-one (81%) (22/27) of patients were able to be maintained at less than 1% isoflurane. Patients were monitored with pulse ox, blood pressure, EKG, temperature, RR, HR with a multiparameter monitor (Image 3). Thermoregulation maintained with warming systemm under blanket under patient and forced air patient warming blanketn dorsally.
Calculus, plaque, and malodor scoring and oral exam followed the same procedure as listed for Day 0. Scoring was performed by the same grader and recording team.
Intra-oral photos were taken of the buccal surfaces of the left and right sides of each subject with check retraction (Images 2-9). Anesthesia records were maintained and recorded parameters every 5 minutes. Once grading and scoring was complete, a dental prophylaxis with periodontal probing and charting was performed by a registered technician or board certified veterinary dentist including periodontal probing, charting, subgingival and supragingival scaling and polishing. Owners had the option of additional imaging and treatment of pathology under the same anesthesia. After completion of the dental prophylaxis and any additional radiographs or treatments elected, the patients were transferred to a padded recovery cage, intubated until swallow reflex returned and monitored until standing and sternal.
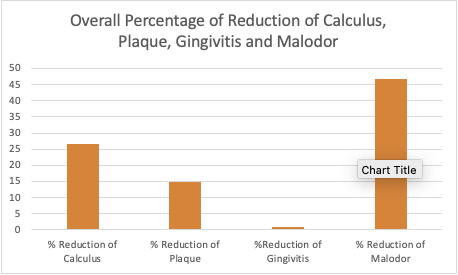
Using a paired t-test there was a statistically significant difference in calculus between day 0 and day 60 (p<0.00001). There was a statistically significant difference in plaque between day 0 and day 60 (p<0.00001).
There was also a statistically significant difference in malodor between day 0 and day 60 (p<0.00001). There was not a statistically significant difference in gingivitis between day 0 and day 60 (p=0.3302).
There was an overall percentage reduction of calculus of 26.6%, plaque of 14.2%, gingivitis 0.99%, and malodor 46.71% (Chart 1)
Halimeter readings were reported in parts per billion (ppb). VSC average reading on Day 0 at 136.93 ppb. After 60 consecutive days of the daily dental chew, the Halimeter average reading was 66.33 ppb over the 27 dogs.
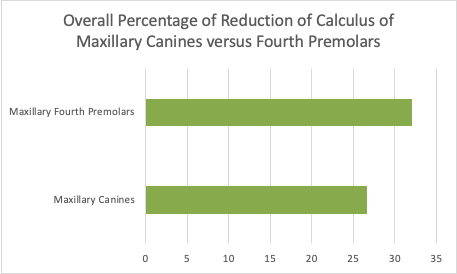
All dogs included in the study ingested the treat without any known adverse events. From Day 0 to Day 60 scoring there was an average weight gain of 1.05 lbs (0.48 kg). Diet was not adjusted for the additional calories from the chew (69kcal/medium treat) while in the study so increased weight was not surprising. The honeycomb shaped dental treat was more efficacious in removing calculus from maxillary fourth premolars than canines, consistent with the functionality of the tooth types and shapes with premolars and molars serving for chewing and grinding (Chart 2).
Client compliance with home care such as tooth brushing has been documented to be low.2,10 Veterinary dental education is clearly needed to increase client compliance. In order to instruct clients in the best practices for oral hygiene and maintenance of periodontal health, education of veterinarians in the college of veterinary medicine curriculum in the pathophysiology of periodontal disease, prevention and treatment is critical. The close, daily interaction of veterinary technicians, nurses, and team members with dog owners/care givers necessitates increased education of these team members and tools to effectively communicate and educate the pet owning public that the oral cavity needs preventative care with the same attention given to dermatological, cardiovascular, and gastrointestinal disease in comprehensive veterinary care.10
Hennet et al. found a significant correlation between heavier calculus on maxillary fourth premolars, calculus indices of 2-3 and increased VSC reading in the presence of halitosis. A significant correlation was also found between increased plaque indices and increased VSC readings. Hennet concluded VSC readings could be used to determine effectiveness of dental hygiene products.11 The link between VSCs and periodontal disease due to possible collagen destruction and membrane permeability in dogs may provide areas of new research and future studies are needed.6,12,13 Professional periodontal therapy with a dental prophylaxis has been shown to reduce malodor for up to 3 months in the dog14,15. Studies in humans have used organoleptic measurements, halimeters, and gas chromatography to measure VSCs.6,7 Previous studies have examined gingivitis, plaque, calculus, and halitosis in toy-breed dogs over 9 weeks.16
Decreased volatile sulfur compounds (VSCs) involved in canine halitosis are hydrogen sulfide (H2S) and methyl mercaptan (CH3SH). These volatile sulfur compounds are byproducts of microbial metabolism and breakdown of proteins. Gram negative anaerobic bacteria have been associated with VSCs.17,18 Gram-negative bacteria (Bacteroides forsythus, Porphyromonas gingivalis, Actinobacillus actinomycetemcomitans, and Prevotella intermedia) have been implicated in the production of VSCs originating from substrates in food. VSCs have also been previously related to the breakdown of food and oral cells, proteins, and bacterial byproducts. 7,18 In humans, VSCs can be decreased more than 50% with tongue scraping.19 Tongue coating scores (TCS scores) have had significant (P<0.001) linear correlation with VSC levels.20 In human studies, methods of controlling halitosis include mechanical debridement, brushing dentition with and without dentifrice/toothpaste, chewing gum, and tongue scraping. Other methods of controlling halitosis target chemical control with deodorizing solutions, topical application of rinses or gels, mouth rinses, tablets, and a combination of these interventions.21 Some authors have noted that sulfur compounds have shown to increase the permeability of the oral mucosa allowing substances such as endotoxins and prostaglandins to penetrate the tissue barrier.22 Research has demonstrated that the change in ingredients of diet, kibble, or chew texture can decrease the level of canine calculus and oral malodor by trained organoleptic evaluation and the use of a portable monitor to measure sulfur compounds.1,23 A study with ten beagles showed significant correlation with organoleptic scoring of halitosis with gingivitis, furcation bone loss, and periodontal probing depths.24
Uniquely designed daily oral hygiene chews that “scrape the surface bacteria from the tongue” may aid in control of periodontal disease. More studies are required to evaluate the bacterial colonization of the canine tongue and its contribution to periodontal disease. Brushing by owners usually does not involve the lingual or palatal surfaces of teeth or the tongue thus home care routines that involve tools and treats that remove plaque from teeth and tongue surfaces may provide more efficacious means of controlling malodor and or periodontal disease. 22 The chew used in this study showed reduction in malodor of all study participants. It could be attributed to “flossing action” and perhaps tongue “scrapping action.”
The Turesky plaque index using a disclosing solution like basic fuchsin dye was not performed on Day 0 due to sedated examination of client owned dogs. The thickness of plaque with dye was not scored at the second visit since the Day 0 data point were not achieved. Methodologies have been described and modified to measure plaque in dogs. The modified Logan and Boyce plaque index was used dividing the crown into horizontal divisions without the intensity evaluation of disclosing dye.25
Plaque components including the microbiota is complex and little research is available on the bacterial species and plaque formation on newly erupted teeth in dogs. In humans, the microbiota and oral environment more complex during the period of tooth eruption. The plaque microbiota forms as early as 12 months after birth.26
Gingivitis scores did not show significant improvement in this study similar to longer term studies where a daily hygiene chew was given. They showed no considerable effect compared to dogs who did not receive a daily chew at the 21-month scoring, but earlier showed a significant effect.5 Mechanical removal of plaque in the dog with daily brushing has been demonstrated to control periodontal disease and brushing has been shown to be effective in controlling plaque and calculus build-up.28 Other limitations of this study include the lack of double blinded scoring and patients entering the study with various degrees of calculus, measured against their own baseline.
The dogs’ canine tooth has an anatomical curvature for apprehending prey and advancing into the prey as prey moves forward to escape. Additional studies and research into chew shape that would allow penetration into a chew to remove marginal plaque and calculus further apical on canine teeth may benefit more morphology-specific areas where calculus begins to form. Tooth morphology, perhaps two different types of treats may be warranted to cleanse the different areas of the teeth as brushing and flossing aid in control of periodontal disease in human subjects.
There are factors of anatomical differences found among dogs including varying occlusions, crowding, root and crown anatomy, pre-existing attachment loss. There are factors of host behavioral patterns like mastication or lack there-of, length of time of mastication, and location of mastication (side preference). Diet and edible treats and chews can affect plaque and calculus with size, texture and chemical composition design. Non-edible oral devices(toys) may also provide mechanical influence. There are host-specific factors like salivary secretion volumes, viscosity, composition, plaque composition, variety in bacterial communities, host immune response, and other yet-to-be determined genetic influences; all contribute to individualized challenges to controlling periodontal disease.4,23,27
Understanding periodontal disease is affected by many factors can help educate owners in caring for their pet’s oral health: anatomical, behavioral, edible and non-edible dental aids, and host specific factors. Knowing the factors that the owner may not be able to control (genetics, host factors) may aid in what outcomes the clients can influence like edible and non-edible dental aids and home care like brushing or water additives.28
Traditionally veterinary dental focused study designs have been cross-over “clean mouth” studies where dogs begin with clean tooth surfaces then are fed a dental diet or daily dental treat, or application of chemicals to tooth surface and evaluated over a specific time period. The control and treatment groups are then switched or “crossed over” and the study repeated.16 Studies are commonly designed with research beagles or focused on one breed for uniformity. There are many studies evaluating the efficacy of dental hygiene chews and other methods of plaque control in research canines housed in research facilities that use a cross over trial design of plaque and calculus accumulation over the duration of 7 days, 21 days, 28 days, 14 weeks, 16 weeks, 63 weeks, and 21 months, but not many studies with years of hardened mature calculus. 5,8,16,23,27,29,30,31,32 The variance of +/- 10 days for the second evaluation may have underestimated the potential of reduction of calculus, plaque, and malodor.
This study is novel due to the use of over 25 breeds of client-owned canines in their normal home environments with mature plaque and hardened calculus of more than 4.1 years evaluated after 60 days of a daily dental chew.
Periodontal disease in dogs is common.33 Client compliance with oral hygiene and oral care for pets is low. Clients should be offered methods to reduce calculus, plaque, gingivitis, and resulting halitosis that are time efficient, cost-effective, and easy to administer between annual preventative dental prophylaxis with the goal to move into maintenance phase of managing periodontal disease. Use of this honeycomb shaped daily dental chew significantly reduced calculus, plaque and associated malodor in dogs when fed consecutively for 60 days.
Pet’s Best Life provided funding for study.
Study conducted with client-owned dogs at Companion Animal Dentistry of Kansas City, R&D Division.









Highlights: Giant breeds are considered breeds that weigh over 90 pounds. Caring for and raising a giant-breed dog requires space, training, and attention to your dog’s special needs. Giant breeds

Highlights: Many breeds of dogs fall into the “large breed” category. Learning to care for these dogs is essential in protecting their longevity and healthspan. Larger dogs tend to have

Highlights: You love your dog, but why are they always looking at you? Dogs may stare at their humans for attention, food, or other reasons. Learning what they need when

Always feed the right treat size for your dog’s weight category. Always supervise your dog when feeding treats. This product is an adult only dog treat. Always provide ample fresh water for your dog.
Type anything...
We use cookies to provide you the best possible experience on our website. You consent to the usage of cookies by continuing to view our website. See our Privacy Notice for more information.